The adductor injury in athletes – we clarify: from etiology to treatment! Groin injuries are particularly common among football players. They account for approximately 9-16% of all football injuries. Diagnosing and treating this type of injury is very complicated for medical experts because there are many inserts and structures in this area that can be a source of pain. Other problems include the high relapse rate, the long break from competition, the unclear prognosis and the long-term symptoms.
Data shows that 69% of groin injuries in soccer players are related to the adductors. If the associated problems persist for a long time, athletes usually have to wait a relatively long time before they can resume their sport. 
An adductor strain, or injury to the adductor muscles, is a common cause of thigh and groin pain, particularly in athletes and elite athletes due to the stress, volume, and strain of training.
Function and structure of the adductor muscles
The adductor complex consists of three adductors (M. longus, M. magnus and M. brevis). The adductor longus is most commonly injured. The main job of these three muscles is to cause adduction of the thigh. The adductor longus is involved in the medial rotation of the thigh
Understanding adductor anatomy
The adductor magnus has an attachment to the ischial tuberosity that gives it the ability to extend the hip. Sometimes when the gluteus maximus (Gmax) is too weak, the adductor magnus and hamstring can assist the Gmax in hip extension. This is very dangerous for the adductor magnus because this type of movement requires a large amount of force that should normally be applied by the Gmax. This exposes the adductor magnus to other injuries.
When the open chain is activated, the main function of the adductor complex is to adduct the hip. When activated with a closed chain, they help stabilize the pelvis and lower extremities during the stance phase of walking or running. They also have secondary functions such as hip flexion and rotation.
Etiology of adductor injuries
The most common sports in which an adductor strain occurs are soccer, hockey, football, tennis, baseball and basketball. Risk factors include a previous hip or groin injury, which is likely to pose the greatest risk, as well as:
the age
- Weakness of the adductor muscle group
- Muscle fatigue, limited range of motion
- insufficient stretching of the adductor muscle complex
- Biomechanical abnormalities such as excessive pronation or leg length discrepancy may also contribute
A sudden change in direction results in rapid adduction of the hip against an abduction force, putting too much strain on the tendon. The most common mechanism of injury is sudden acceleration while sprinting, while jumping or overstretching the adductor tendon are less common causes.

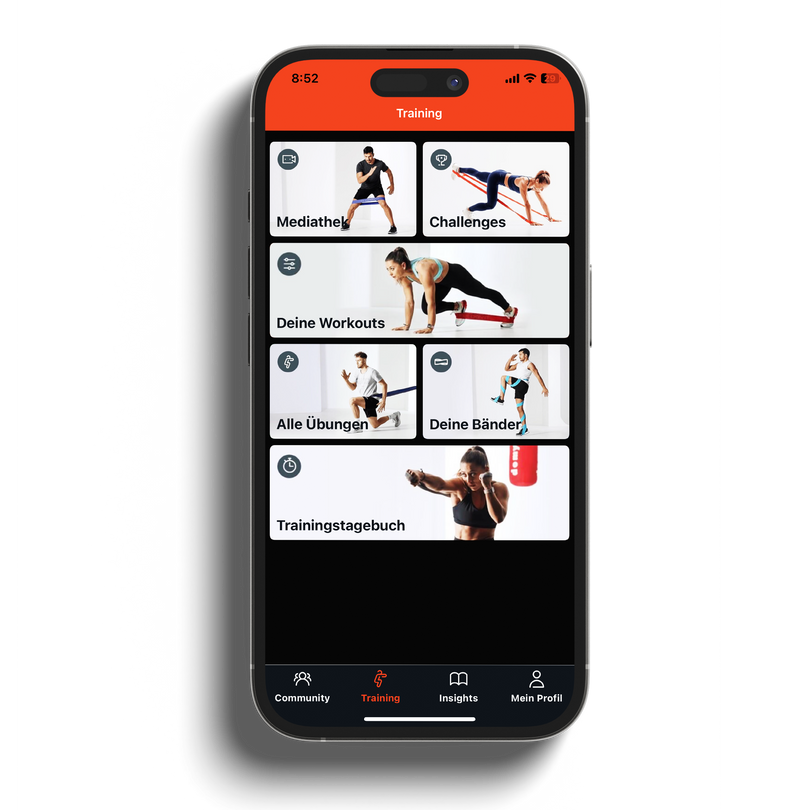
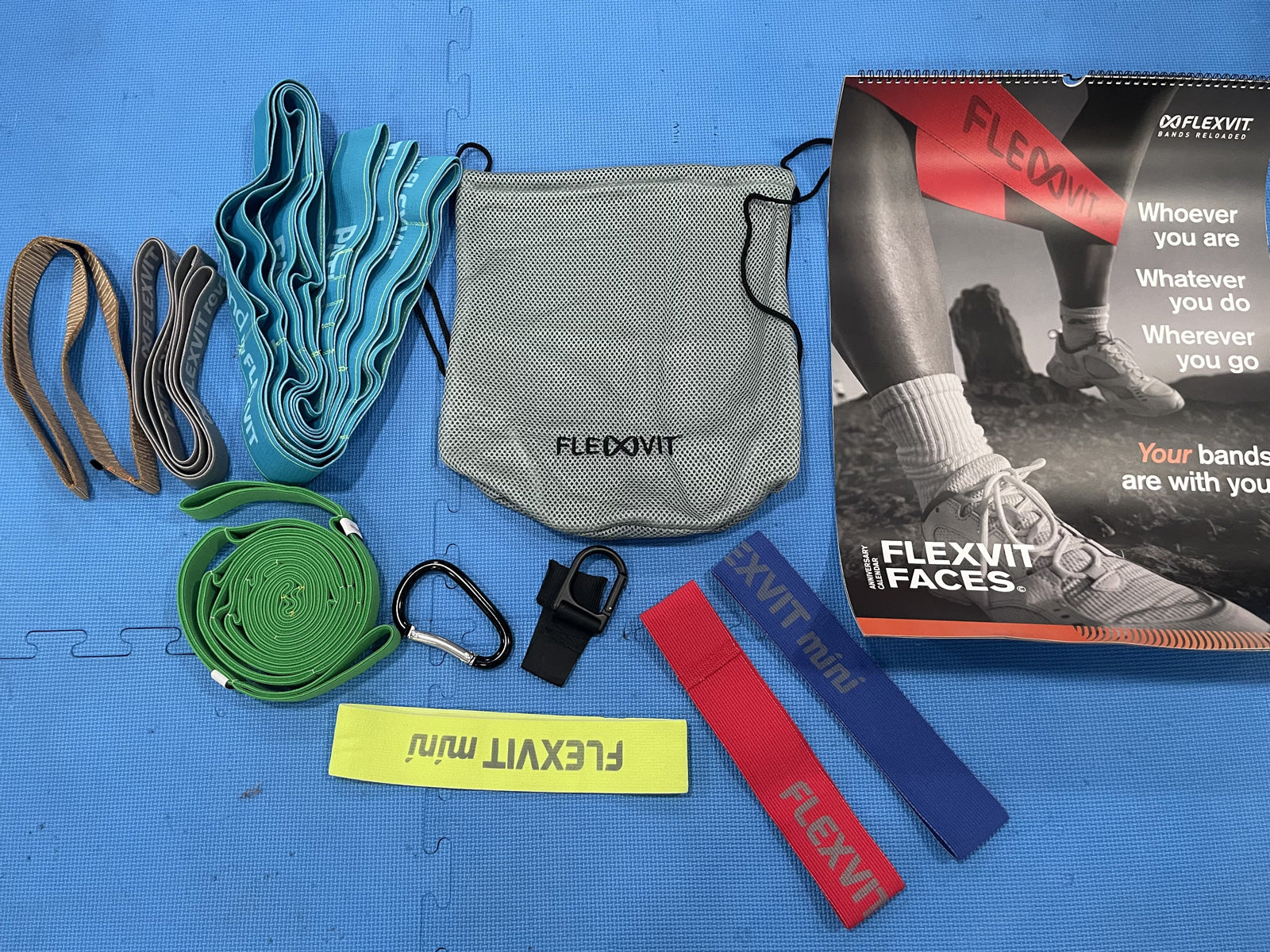
With our fitness and resistance bands you can prevent injuries in sports - discover our training bands now & prepare yourself perfectly for your upcoming training or competition!
Clinical aspect
The first method of choice if an adductor strain is suspected is an X-ray examination. In most cases, the appearance is normal unless the injury has resulted in a separation at the insertion. These types of images can help the medical team evaluate or rule out other types of injuries such as osteitis pubis or stress fractures.
Ultrasound (US) can provide good information about the severity of the injury. The tendon, bone attachments and ligaments can be quickly assessed using US. This can be used to determine the area and extent of the injury, but also to track the healing of the injury site and the effect of treatment.
If we want to look deeper and more precisely, an MRI can be done. This can be used to detect muscle edema and bleeding at the injury site. Bone injuries can also be better recognized on an MRI.

Rehabilitation after an adductor injury
Adductor group rehabilitation must focus on strengthening, stretching, range of motion exercises, and sport-specific drills to allow for a gradual return to play (RTP). The modified Holmich protocol developed by Yousefzadeh et al. Proposed in 2018, appears to be an effective way of rehabilitation. The result of treatment by this protocol was an RTP of 86.6% after 12.06 weeks in the athletes. The factors responsible for the better results compared to the original Holmich protocol are likely due to the fact that the modified protocol includes:
- Strengthening with elastic bands and emphasizing time under tension
- Use of exercises to stabilize the torso
- High-intensity eccentric training for the adductor complex
- Stretching the adductors
Stretching the adductor group is also important because it allows better restructuring of the fibers in the right direction thanks to the mechanical force exerted by stretching.
Here is an example of stretching the adductors with FLEXVIT® bands:
Here is an example of an adductor strain rehabilitation exercise using FLEXVIT® bands:
Dealing with pain from an adductor injury
Physical therapy:
Massage and electrotherapy can be used at the beginning of rehabilitation for pain relief and during the exercises of the rehabilitation program for recovery.
Movement:
Pain can be relieved with isometric exercises. In fact, isometric contraction has a pain-relieving effect due to a physiological phenomenon called corticomuscular inhibition. Light contractions against resistance (e.g. the physical therapist's hands) in a shortened position of the adductor muscle can be performed at the beginning of treatment. Of course, this depends on the athlete's feelings.
Then you can use isometric strength in conjunction with e.g. B. continue this sitting exercise:

About the authors:
Antoine Fréchaud (left) and Nathan Touati (right) run NeuroXtrain, a website specializing in writing articles and various content on the topics of sports science, athlete rehabilitation, performance and new technologies for athlete health. 
Instagram | Facebook | LinkedIn

DISCLAIMER: This content (the description, images and videos) does not constitute medical advice or treatment plan and is intended for general educational and demonstration purposes only. This content should not be used for self-diagnosis or self-treatment of any health, medical or physical condition. This content cannot replace professional advice or medical advice. To be on the safe side, before using exercises to combat specific complaints, you should always consult a doctor or physiotherapist.
Effectively prevent injuries now – with the resistance bands from FLEXVIT!